Saturday, August 24, 2019
My Last Manic Episode - My Theory
Been thinking that my last manic episode- April/May this year- may have been started by my best friend dying on April 2nd. It was a couple weeks later that I started haviing noticable symptoms of mania. From there it just got worse until I contacted my team and was drugged into submission with Seroquel.
Tuesday, August 20, 2019
Psychology Today: Robin Williams Bipolar
Not Depression But Bipolar- Robin Williams
Yup- we knew it: He was Bipolar!
(Text copied in case link dies.)
Not "Depression": Manic-Depression and Robin Williams
A deadly disease, whether we accept it or not
Posted Aug 13, 2014
Was it “depression” that killed Robin Williams, as most media reports say? Or depression mixed with alcohol and drugs. But “depression” isn’t a diagnosis or a disease; like fever, it’s a set of symptoms that can happen in various diseases.
The disease was manic-depression, or bipolar illness, as some reportsacknowledge; depression occurred as part of that disease, and, in all likelihood, it led to Williams’ suicide. Alcohol and/or drugs may have precipitated the timing and the exact end, but the disease which afflicted him, over and over with repeated mood episodes, was manic-depression.
article continues after advertisement
“Depression” is somewhat acceptable; manic-depression is still mostly taboo. Even mental health clinicians, including many on the PT site, downplay or denigrate it.
But it exists; it provides great gifts; and it kills.
The gifts: creativity in mania certainly helps comedians and actors; the mind runs in a million different directions, and new and funny and smart ideas pour out. Williams was a walking manic episode in many of his interviews and skits. Sometimes a person can have mild to moderate manic symptoms all the time, as part of his or her personality, called “hyperthymic” temperament, the opposite of “dysthymic” temperament. In keeping with the stigma and discrimination against bipolar illness, dysthymia is well-known and part of the DSM nosology; hyperthymia was never included in DSM systems, and is little known among mental health clinicians, much less the larger public.
Many persons with manic-depressive illness have hyperthymic temperament all the time – so they’re creative and productive and funny, and sometimes famous – and then they have repeated depressive episodes, usually lasting weeks to months, usually happening once a year or two – and, in about one in ten persons, leading to suicide.
So Robin Williams’ “depression” should be called what it was: manic-depression. And we need to start taking this bipolar illness more seriously and respectfully, and acknowledging its existence, and treating it correctly –rather than misnaming it and mistreating it (as happens with “depression”, where antidepressants often worsen the bipolar illness, sometimes leading to suicide), or, worse, simply ignoring it.
article continues after advertisement
Tragedy is sad if not preventable, but truly terrible when a cure exists, such as lithium, which is proven to prevent suicide in multiple gold-standard randomized studies. And, more importantly, it is the ONLY medication proven to prevent suicide in randomized studies.
The cure exists; the diagnosis can be made. The real tragedy is that we pretend the diagnosis doesn’t exist.
Williams, Philip Seymour Hoffman, Amy Winehouse - and in the past, Kurt Cobain and others.
The tragedies will never end –as with all medical tragedies, like the millions of women who died in childbirth for millennia – until scientific and medical professions take a disease seriously. Only then can it be identified - and cures given.
Saturday, August 17, 2019
An Unquiet Mind (By Kay Redfield Jamison)
I just finished it. My impressions: She is a remarkable writer- several $15 dollar words that I had to look up! That's unusual for me. She explained things that were in terms I could understand - maybe because Ive got "it", too? Her insistance of calling it "manic depressive illness"; she even goes on to explain why. To me, "manic depression" describes part of it- but there's so much MORE to it. Bipolar tells you there are at least two opposite ends of the disease but leaves room for all the little inbetween bits- such as delusions, hallucinations, and paranoia. All in all, I loved the book. I have respect for her journey. Likely, the best memoir I've read about bipolar. I am left with a feeling of hope and maybe I don't "need" to know what's "worse" than what I've already experienced in my life re bipolar.
Monday, August 12, 2019
Everybody Wants Me to Take My Meds
My liver doctor- even after he said my liver issues likely started with psych meds- told me to not stop taking my psych meds. That was last Wednesday. Today my mom told me to not stop them, too. Today he said I need a biopsy and I can be sedated if I want. I hope they don't use Ativan. I will need somebody to drive me. My mom even said I should take my meds because "we don't need that". Meh! I was upset today. I need a special diet and was told the diet clinic they want me to go to is $700 for 10 weeks! 
 The dr also told me that some of the tests say I have cihrrosis and some say I do not so I need a biopsy. All of this because I made the choice to take psych meds. Yup. They started this disaster. I wrote about this in my blog this past Spring of what COULD happen with references and yup! My liver doctor confirmed it this past Wednesday- psych meds cause obesity which causes metabolic syndrome which causes. fatty liver which causes cihrrosis. I found the metabolic syndrome diet online and it makes sense- hope to get rid of high blood pressure high cholesterol, pre-diabetes.... And everybody wants me to stay on the drugs that are destroying me! I spent part of today crying because I'm going to die an early death if I can't pull off a miracle here. And my doctors- primary and pdoc- just sat and watched it all happen. I found a lot of info online about the metabolic diet- Its what they are teaching in that class. I also left a message for my primary- maybe I can see a regular nutrition a few time- I know my insurance will cover that.
The dr also told me that some of the tests say I have cihrrosis and some say I do not so I need a biopsy. All of this because I made the choice to take psych meds. Yup. They started this disaster. I wrote about this in my blog this past Spring of what COULD happen with references and yup! My liver doctor confirmed it this past Wednesday- psych meds cause obesity which causes metabolic syndrome which causes. fatty liver which causes cihrrosis. I found the metabolic syndrome diet online and it makes sense- hope to get rid of high blood pressure high cholesterol, pre-diabetes.... And everybody wants me to stay on the drugs that are destroying me! I spent part of today crying because I'm going to die an early death if I can't pull off a miracle here. And my doctors- primary and pdoc- just sat and watched it all happen. I found a lot of info online about the metabolic diet- Its what they are teaching in that class. I also left a message for my primary- maybe I can see a regular nutrition a few time- I know my insurance will cover that.

 The dr also told me that some of the tests say I have cihrrosis and some say I do not so I need a biopsy. All of this because I made the choice to take psych meds. Yup. They started this disaster. I wrote about this in my blog this past Spring of what COULD happen with references and yup! My liver doctor confirmed it this past Wednesday- psych meds cause obesity which causes metabolic syndrome which causes. fatty liver which causes cihrrosis. I found the metabolic syndrome diet online and it makes sense- hope to get rid of high blood pressure high cholesterol, pre-diabetes.... And everybody wants me to stay on the drugs that are destroying me! I spent part of today crying because I'm going to die an early death if I can't pull off a miracle here. And my doctors- primary and pdoc- just sat and watched it all happen. I found a lot of info online about the metabolic diet- Its what they are teaching in that class. I also left a message for my primary- maybe I can see a regular nutrition a few time- I know my insurance will cover that.
The dr also told me that some of the tests say I have cihrrosis and some say I do not so I need a biopsy. All of this because I made the choice to take psych meds. Yup. They started this disaster. I wrote about this in my blog this past Spring of what COULD happen with references and yup! My liver doctor confirmed it this past Wednesday- psych meds cause obesity which causes metabolic syndrome which causes. fatty liver which causes cihrrosis. I found the metabolic syndrome diet online and it makes sense- hope to get rid of high blood pressure high cholesterol, pre-diabetes.... And everybody wants me to stay on the drugs that are destroying me! I spent part of today crying because I'm going to die an early death if I can't pull off a miracle here. And my doctors- primary and pdoc- just sat and watched it all happen. I found a lot of info online about the metabolic diet- Its what they are teaching in that class. I also left a message for my primary- maybe I can see a regular nutrition a few time- I know my insurance will cover that.
Thursday, August 8, 2019
Maybe it's Too Late
I want to wean off Seroquel- im only on 150 as it is. Same goes for the 2.5 of Haldol and 3 of Rexulti. If I'm gonna die soon so be it but why add fuel to the fire? Maybe the damage has been done and its too late
Antipsychotics killing me!
I am so sick of this whole thing. I want off all psych drugs! They can treat me in the psych hospital but maintenance drugs? Nope. Im also sick of feeling inferior with my "bad brain". This is not who I was supposed to be! Sick! And I am more afraid of liver failure than I am of mania. But we are talking YEARS of cumulative damage!! The doctors tried not to scare me today but fatty liver has turned to some hardening! And they added STAT same DAY tests- ultrasound and another scan test. What's next? Cirrhosis- THAT'S what!
Wednesday, August 7, 2019
Bipolar is a physical illness- original study!
https://www.nature.com/articles/mp201773
Original Article! (Click for full study.)
Abstract: Despite decades of research, the pathophysiology of bipolar disorder (BD) is still not well understood. Structural brain differences have been associated with BD, but results from neuroimaging studies have been inconsistent. To address this, we performed the largest study to date of cortical gray matter thickness and surface area measures from brain magnetic resonance imaging scans of 6503 individuals including 1837 unrelated adults with BD and 2582 unrelated healthy controls for group differences while also examining the effects of commonly prescribed medications, age of illness onset, history of psychosis, mood state, age and sex differences on cortical regions. In BD, cortical gray matter was thinner in frontal, temporal and parietal regions of both brain hemispheres. BD had the strongest effects on left pars opercularis (Cohen’s d=−0.293; P=1.71 × 10−21), left fusiform gyrus (d=−0.288; P=8.25 × 10−21) and left rostral middle frontal cortex (d=−0.276; P=2.99 × 10−19). Longer duration of illness (after accounting for age at the time of scanning) was associated with reduced cortical thickness in frontal, medial parietal and occipital regions. We found that several commonly prescribed medications, including lithium, antiepileptic and antipsychotic treatment showed significant associations with cortical thickness and surface area, even after accounting for patients who received multiple medications. We found evidence of reduced cortical surface area associated with a history of psychosis but no associations with mood state at the time of scanning. Our analysis revealed previously undetected associations and provides an extensive analysis of potential confounding variables in neuroimaging studies of BD.
Sunday, August 4, 2019
Bipolar IS a Physical Illness!
https://www.psychologytoday.com/us/blog/the-athletes-way/201705/new-mri-study-leads-roadmap-bipolar-brainsNew MRI Study Leads to Roadmap of Bipolar Brains | Psychology Today
-
Personality
Personal Growth
Relationships
Family Life
View Help Index
Do I Need Help?
Recently Diagnosed?
Talk to Someone
Mental Health
Protect Yourself from Emotional Contagion
Whether it’s joy or anger, we’re wired to catch and spread emotions. Here's how to inoculate ourselves against negative ones.
Essential Reads
Trending Topics
News
New MRI Study Leads to Roadmap of Bipolar Brains
International MRI meta-analysis creates first global map of bipolar disorder.
Posted May 02, 2017
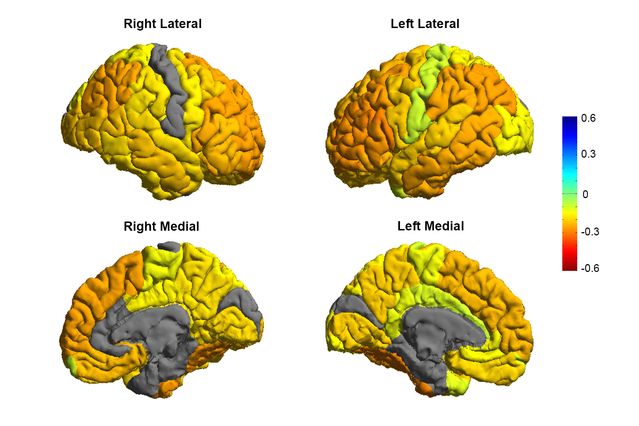
Bipolar patients tend to have gray matter reductions in frontal brain regions involved in self-control (orange colors), while sensory and visual regions are normal (gray colors).
Source: Courtesy of the ENIGMA Bipolar Consortium/Derrek Hibar et al.
A new landmark study—which is the largest meta-analysis of MRI brain imaging to date—has identified specific brain abnormalities in gray matter volumes of people with bipolar disorder(BD) and created the first “roadmap” of key brain regions underlying the neurobiology of BD. These findings were published May 2 online ahead of print in the journal Molecular Psychiatry.
Senior author of this study, Ole Andreassen, a researcher and professor at the Norwegian Centre for Mental Disorders Research at the University of Oslo, said in a statement, "We created the first global map of bipolar disorder and how it affects the brain, resolving years of uncertainty on how people's brains differ when they have this severe illness."
The new roadmap for the bipolar disorder shows that adults with BD tend to have widespread bilateral patterns of reduced cortical thickness in frontal, temporal, and parietal regions. In adult patients diagnosed with bipolar disorder, the ventrolateral prefrontal cortex (VLPFC) displayed the most dramatic reduction in cortical thickness. In adolescents/young adults, the researchers found reduced thickness and surface area in the supramarginal gyrus and insula (respectively) associated with BD. Notably, previous functional brain imaging (fMRI) studies have shown increased activity in the VLPFC in remitted BD during emotion regulation.
article continues after advertisement
The World Health Organization estimates that Bipolar disorder (sometimes referred to as manic-depression) affects about 60 million people globally or roughly one percent of the population. BD can be a debilitating psychiatric disorder. Bipolar disorder is generally characterized by extreme mood swings—which can range from severe lows and major depressive episodes (MDE) to hypomania. Until recently, researchers have struggled to pinpoint specific neurobiological mechanisms of the disorder, partly due to technological limitations and lack of high-quality brain scans.
The monumental amount of MRI data included in the latest BD meta-analysis comes from an international collective called “ENIGMA” (Enhancing Neuro Imaging Genetics Through Meta Analysis). This cohort of scientists uses the University of Southern California (USC), Los Angeles as their home base and spans 76 centers and includes 26 different research groups around the world. The latest ENIGMA meta-analysis of bipolar of MRI included a total of 6,503 individuals (2,447 adults with BD and 4,056 healthy controls).
article continues after advertisement
The ENIGMA researchers also examined the effects of commonly used prescription medications (such as lithium) to treat bipolar disorders as well as other BD factors such as the age of initial onset, familial history of psychosis, and sexdifferences within various cortical regions of the cerebral cortex.
Lithium was approved in the 1970s by the FDA and remains one of the most widely used medications for treating bipolar disorder. Lithium helps reduce the severity and frequency of manic episodes. But psychopharmacologists and psychiatrists still don't understand exactly how lithium works to help patients with bipolar disorder. That said, the latest brain scans offer some clues that help explain why lithium works by increasing gray matter volume in affected areas.
"These are important clues as to where to look in the brain for therapeutic effects of these drugs," Derrek Hibar, first author of the paper and a professor at the USC Stevens Neuroimaging and Informatics Institute said in a statement. Hibar was a visiting researcher at the University of Oslo when this meta-analysis was conducted.
article continues after advertisement
The ENIGMA researchers believe that mapping the brain regions associated with bipolar disorder is of great value for early detection and prevention. Paul Thompson, director of the ENIGMA consortium and another co-author of the study, concluded, "This new map of the bipolar brain gives us a roadmap of where to look for treatment effects. By bringing together psychiatrists worldwide, we now have a new source of power to discover treatments that improve patients' lives."
Future ENIGMA research will test how well different medications and treatments can shift or modify these brain measures as well as improve symptoms and clinical outcomes for BD patients.
How Is the Cerebellum Linked to Bipolar Disorder?
In a 2016 Psychology Today blog post, I reported on a groundbreaking study by researchers at the University of Iowa who used a state-of-the-art MRI technique to identify a correlation between abnormalities of the cerebellum, differences in cerebral white matter, and bipolar disorder. These MRI findings from UI dovetail with the latest ENIGMA meta-analysis by Habir et al.
article continues after advertisement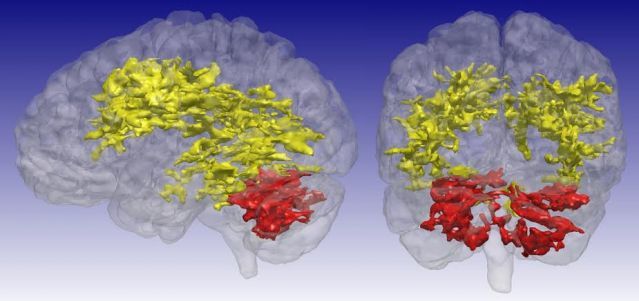
Using a revolutionary MRI technique that is sensitive to certain byproducts of cell metabolism, University of Iowa researchers discovered previously unrecognized differences in the brains of patients with bipolar disorder. The T1rho MRI scans showed brain regions of elevated signal in participants with bipolar disorder compared with study participants who did not have bipolar disorder. The primary regions of difference are the cerebral white matter (yellow) and the cerebellum (red).
Source: Courtesy of University of Iowa
After reading the new ENIGMA meta-analysis this morning, I was curious to learn if the co-authors of the new study had any insights about the role that the cerebellum might play in bipolar disorder. So, I sent the enigma corresponding author in Norway an email. I wrote:
"Dear Ole Andreassen, As I was reading the results of your latest meta-analysis, the potential cerebellar link to bipolar disorder seemed like an "elephant in the room" that I have a hunch might somehow be correlated to your findings.I know that so much of the research on the cerebellum is in its infancy and any conclusions would be speculative at this point. That being said, I'm always curious to hear expert opinions on the role that the cerebellum might play in cognitionand mental disorders. Regarding next steps for creating a "whole-brain" roadmap for BD that includes the cerebellum, I was wondering if you could answer a few questions? I would love to share your answers with my Psychology Today readers."
My questions for Ole Andreassen were as follows:
"I’m curious if your MRI meta-analysis of 2,447 adults with bipolar disorder was able to include any brain mapping studies that looked at the possible role of gray matter volume or white matter integrity in the cerebellum? If so, do you have a hypothesis about the link between cerebellar gray matter brain volumes or the integrity of white matter tracts in specific regions or hemispheres of the cerebellum (such as lobule VIIb) being linked to mental disorders?Also, based on your extensive knowledge of MRI neuroimaging, do you think it's possible that the thinning of gray matter in the cerebral cortex of patients with bipolar disorder in regions of the frontal and temporal lobes might somehow be linked to changes in gray matter volumes within specific cerebellar lobules or microzones?"
Ole Andreassen responded: "Thanks for your insightful questions. We are aware of the lack of information about cerebellum in these analysis of brain abnormalities in bipolar disorder, as well as in other ENIGMA studies of, for example, schizophrenia. I agree that this is an important factor that currently is missing in these large multi centre brain MRI analysis.
Andreassen continued, "To show our interest for the role of cerebellum in severe mental disorders, we have a paper in press from our centre specifically targeting cerebellum in MRI studies of severe mental disorders. I have Cc Lars Westlye and Torgeir Moberget who are leading that effort and have some exciting hypothesis about the specific cerebrum-cerebellum networks. They have more knowledge about the specific questions related to cerebellum."
A few minutes later, Lars Westlye wrote me saying, "Dear Chris, Thanks for your interest. Please find attached our in press paper on cerebellar structure in schizophrenia, Torgeir (Cc) is lead author. The paper is embargoed until publication date, which will probably be within a few weeks."
Cerebellar research is a trailblazing new frontier of neuroscientific study. I will be providing any updates on the aforementioned embargoed paper by Torgeir et al. as soon as possible. Hopefully, these findings will help to answer some of the enigmatic riddles of how cerebellar volume and cerebello-cerebral structural covariance influences a wide range of mental health disorders. Stay tuned!
References
D.P. Hibar, O. A. Andreassen, et al. Cortical abnormalities in bipolar disorder: an MRI analysis of 6503 individuals from the ENIGMA Bipolar Disorder Working Group. Molecular Psychiatry advance online publication 2 May 2017; doi: 10.1038/mp.2017.73
C P Johnson, R L Follmer, I Oguz, L A Warren, G E Christensen, J G Fiedorowicz, V A Magnotta, J A Wemmie. Brain abnormalities in bipolar disorder detected by quantitative T1p mapping. Molecular Psychiatry, 2015; DOI: 10.1038/mp.2014.157
"Structural Alterations within Cerebellar Circuitry are Associated with General Liability for Common Mental Disorders," Adrienne L. Romer, Annchen R. Knodt, Renate Houts, Bartholomew D. Brigidi, Terrie E. Moffitt, Avshalom Caspi and Ahmad R. Hariri. Molecular Psychiatry, April 11, 2017. DOI: 10.1038/MP.2017.5
advertisement
About the Author
More Posts
Find a Therapist
Get the help you need from a therapist near you–a FREE service from Psychology Today.
Cities:
- Atlanta, GA
- Austin, TX
- Baltimore, MD
- Boston, MA
- Brooklyn, NY
- Charlotte, NC
- Chicago, IL
- Columbus, OH
- Dallas, TX
- Denver, CO
- Detroit, MI
- Houston, TX
- Indianapolis, IN
- Jacksonville, FL
- Las Vegas, NV
- Los Angeles, CA
- Louisville, KY
- Memphis, TN
- Miami, FL
- Milwaukee, WI
- Minneapolis, MN
- Nashville, TN
- New York, NY
- Oakland, CA
- Omaha, NE
- Philadelphia, PA
- Phoenix, AZ
- Pittsburgh, PA
- Portland, OR
- Raleigh, NC
- Sacramento, CA
- Saint Louis, MO
- San Antonio, TX
- San Diego, CA
- San Francisco, CA
- San Jose, CA
- Seattle, WA
- Tucson, AZ
- Washington, DC
Are you a Therapist?
Subscribe to:
Posts (Atom)